Spasticity Learning Center
from HumanPhysiology.Academy
Spasticity 101: injury and recovery
The term Cerebral Palsy (CP) is used to describe any injury of the brain which occurs before 2 years of age. The neurological insult in CP by definition does not worsen. There are many causes of CP, including neonatal stroke, birth trauma, near drowning, non-accidental trauma, and brain ischemia (not enough oxygen to the brain). The neurons (nerve cells) in the brain are damaged, decreasing the ability of the child to control their arms, legs, speech, etc. One, two, three, or four limbs may be involved. Even the ability to see, hear, and feel can be affected. Cognition (intelligence) can also be affected but may be normal.
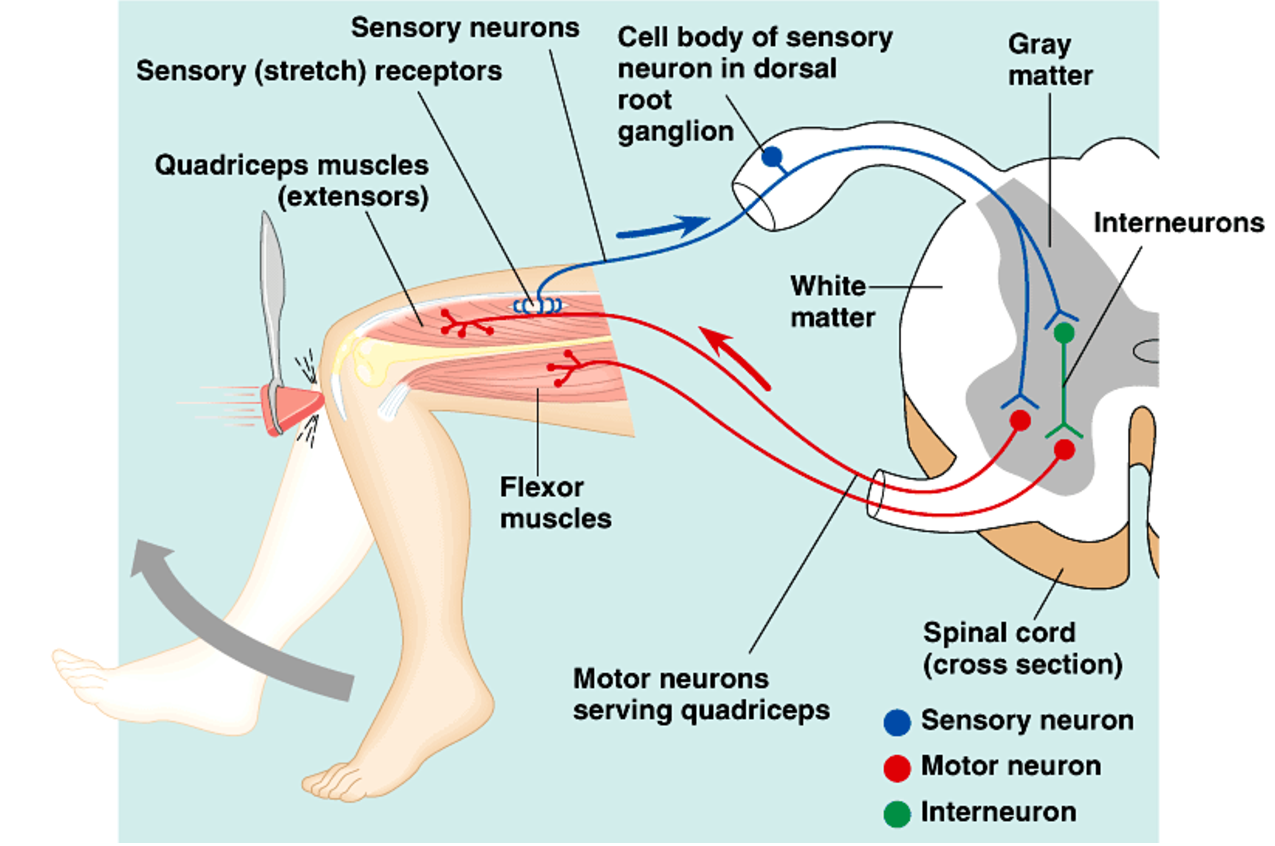
The central nervous system is made up of upper motor neurons in the brain and lower motor neurons in the spinal cord. The upper motor neurons tell the lower motor neurons what to do, and the lower motor neurons directly control the muscles. The lower motor neurons can also be triggered by spinal cord reflexes, which are themselves modulated by stress or excitement, as well as by the upper motor neurons. It is the job of the upper motor neurons in the brain to quiet the lower motor neurons, effectively muting the spinal cord reflexes. When the upper motor neurons in the brain are damaged, as is the case in children with CP or any other brain injury such as stroke or traumatic brain injury, the upper motor neurons are unable to quiet the activity of the lower motor neurons. Without inhibition from the upper motor neurons, the spinal reflexes are unchecked and the lower motor neurons activate muscle contraction with the slightest agitation or stretch of the muscle, a condition known as spasticity.
An understanding of the spinal reflex arc is necessary to understand both how spasticity develops and how we can treat it. The spinal reflex arc is what gives us deep tendon reflexes such as the patellar tendon reflex, and the Hoffman Sign. When a muscle is stretched, spindle fibers within the muscle sense the stretch and send an electrical signal back to the spinal cord, directly activating the lower motor neuron in the anterior horn (the anterior horn cell). An inhibitory signal to the antagonist muscle(s) is sent simultaneously via an interneuron.
Children with CP tend to posture with their elbows, wrists, and fingers bent. This posture is maintained because the lower motor neurons are disinhibited and therefore spastic. If the spasticity is severe, these persistent joint postures over time can lead to joint and muscle contractures, where even passive range of motion is affected. Often, even children who have some ability to actively control their muscles are unable to overcome the spasticity and/or the joint and muscle contractures. Voluntary motion can therefore be limited beyond that which is possible from the remaining functioning upper motor neurons in the brain. Treatment is therefore focused on relieving spasticity and contractures to optimized use of the arm. This is done with a combination of nerve resections and tendon/joint releases.
Spasticity 201: Tendon lengthening, muscle releases, and myotomies
Longstanding spasticity keeps muscles in contracted position, preventing full motion of affected joints. The elbow, for example, is often flexed, as the biceps, brachialis, and brachioradialis muscles overpower the triceps. In some patients, the spasticity is mild enough that they never develop fixed contractures of the elbow. In others, the spasticity is severe enough to prevent even passive elbow extension within a full range of motion. If the elbow is maintained in flexion for even just a few months in a growing child, the muscles that bend the elbow are never stretched, and therefore do not grow to keep up with the growing skeleton. Because the major blood vessels and nerves are also in front of the elbow joint, these likewise do not lengthen sufficiently to allow full motion. Over years, the blood vessels and nerves become the limiting factors in how much the elbow can be straightened, because these cannot be lengthened surgically. Prolonged and diligent therapy may help in stretching arteries and nerves, but this requires a serious commitment from the patient and/or family, and can be painful.
Muscles, however, can be lengthened in a variety of ways. Stretching with therapy and/or serial casting with and without administration of botulinum toxin can help improve passive motion. The addition of botulinum toxin helps decrease muscle strength by blocking the nerve signal from the spinal cord to the muscle. A weaker muscle is less able to resist stretching and serial casting, resulting in potentially more effective therapy. If stretching, splinting, and casting do not resolve the contracture, surgery may be an option to consider. Muscles can be surgically lengthened by 1) fractional lengthening, 2) tendon “Z” lengthening, or 3) muscle origin release (slide). All muscles have an origin (a place where it starts from on a bone or tendon), and a terminal tendon that attaches it to another bone. The muscle is derived from cells that are related to neurons, and the muscle cells retain the electrical conduction properties of their nerve cousins. Muscle cells form long chains called muscle fibers that can stretch and contract. Tendon cells are more closely related to bone cells, and primarily function to create and maintain a matrix of strong collagen fibers oriented along the long axis of the tendon. Collagen is very strong and does not stretch or lengthen very easily, much like a rope. During embryogenesis, the muscle cells fuse with the tendon cells, creating a musculotendinous junction. Because this junction is relatively weak, it usually extends a long distance within the muscle to minimize the chance of rupture.
Fractional lengthening takes advantage of the fact that muscles stretch more than tendon, and is performed by cutting the tendon inside the muscle. The cut tendon ends can no longer resist stretching, and gap open, surrounded by muscle. Within a few weeks, scar forms across the two tendon ends and the muscle adjusts to its new length, recovering its strength. Fractional lengthening is ideal for muscles that have a long internal tendon, and for when only a small amount of lengthening is required.
If more lengthening is needed, the tendon can be lengthened by cutting the tendon along its length into two halves, one attached distally to the bone and the other attached proximally to the muscle. The two halves are allowed to shift past each other and then sewn together in a lengthened state. Because more lengthening is achieve and the muscle is not itself lengthened, “Z” lengthening results in more muscle weakness and may decrease the active arc of motion.
While fractional lengthening and Z lengthening lengthen one muscle at a time, a muscle origin release can target either one muscle or an entire muscle group. One advantage of a muscle slide is that it does not cause any internal damage to the muscles, usually maintaining their strength. Another advantage is that it allows the muscle to find its own resting length, removing any need for intra-operative adjustment of muscle length.
If a muscle is more of a nuisance than it is useful, such as the brachioradialis can be, another option is to cut the muscle entirely (myotomy). A myotomy completely removes any muscle function from that muscle and is not reversible. Therefore, myotomy should be used sparingly and with clear indications.
spasticity 202: Managing spasticity
Spasticity can lead to joint contractures often requiring joint and/or muscle and tendon releases as described in SPASTICITY 201 above. But the underlying cause remains muscle spasticity. Management of spasticity from an early age can prevent joint contractures, requiring less therapy and fewer surgeries throughout life. There are currently many research studies looking at ways to manage spasticity with medications and therapy. Currently, the gold standard is Baclofen delivered directly into the cerebrospinal fluid (intrathecal Baclofen), usually with an implanted pump. Other medications such as Valium or Ativan can be used. These medications do not target any specific muscles, but rather provide a general decrease in the spinal reflex arc. A global decrease in muscle tone is helpful for most children with spasticity regardless of the cause.
If only specific muscles are overly spastic, putting joints out of balance, Botulinum Toxin can be injected into these muscle to temporarily weaken them. Botulinum toxin is made by bacteria called Clostridium Botulinum, and is the most powerful poison known to man. Just 1-2 nanograms per kilogram, if injected, is enough to kill a person. Botulism is the poisoning that can occur from canned foods, and is the reason one should not eat anything from a bloated can. Likewise, jars of food have a pop-up to alert the consumer that if the top is popped, the risk of Botulism is high. However, used sparingly, at about 10-50 units per muscle, Botulinum toxin poses little risk. The toxin permanently binds to the terminal end of the nerve axon and prevents the release of acetylcholine, a neurotransmitter required for signaling the muscle to contract. The result is muscle weakness, breaking the short circuit of the spinal reflex arc. Over the subsequent 3 months, the nerve sprouts new ends form its axon and creates new neuromuscular junctions, recovering muscle function. The effects of Botulinum toxin therefore only last for an average of 2-3 months. Repeat injections 4 times a year can be onerous, expensive, and taxing on the child. They also reduce spasticity by weakening the muscle, reducing the function of the limb in some patients.
More permanent and effective options concentrate on interrupting the spinal reflex arc at the signal from the muscle to the spinal cord level. A selective dorsal rhizotomy (SDR) disconnects the dorsal root ganglion at any particular spinal cord level, preventing most sensory feedback from entering the spinal cord. While more “selective” than Baclofen, in that it only affects the spinal levels where the roots are cut, SDR reduces not just spasticity but also sensation and proprioception (the ability to know where your limb is in space). However, it does not impact strength at all, since none of the signal from the spinal cord to the muscle is interrupted.
By contrast, Selective and Hyper-selective Partial Denervation (SPD or HSPD) is performed close to the muscle, allowing a more targeted spasticity reduction muscle by muscle. In SPD or HSPD, nerve branches to spastic muscles are isolated and split into fascicles, like separating individual fibers from a braided rope. Approximately 2/3rds of the fascicles are removed, leaving 1/3rd behind to power the muscle. These nerve branches are about 60% afferent (carrying signal from the muscle to the spinal cord) and 40% efferent (carrying signal from the spinal cord to the muscle) fibers. A nerve stimulator is used to identify fascicles that have greater afferent component, and to confirm redundancy in the fascicles. Efferent nerve fibers are capable of multiplying within the muscle to power 5 times as many muscle fibers as in their native state. It is therefore possible to remove up to 80% of efferent fibers without losing any muscle strength in the long term. Temporary weakness of the muscle is common as the efferent nerves expand, a process that takes 3-12 months to complete. The afferent (sensory) fibers that are left behind cannot multiply like the efferent (motor) fibers. Since these afferent (sensory) fibers are the start of the reflex arc, removal of 50-80% of these fibers results in a proportional decrease in the spasticity of that muscle. The result in most patients is a noticeable decrease in spasticity without a noticeable loss in strength. Another advantage over less targeted surgical methods is that the feeling of the limb is not compromised.
None of the options discussed above, however, are able to enhance the child’s ability to control the limb. While a decrease in spasticity may be able to uncover hidden function in an antagonist muscle, it cannot restore to brain cells that were lost. Normally, the right brain primarily controls the left side of the body, with most descending nerve fibers crossing within the spinal cord from right to left and left to right. A few fibers do not cross, giving some control of the limb in most patients. Researchers in Shanghai, China therefore spent over a decade developing a new technique for connecting the unaffected side of the brain in hemiplegia to the affected side of the body. The Contralateral C7 (CC7) technique has been in use for many decades for the treatment of brachial plexus nerve injuries. Adapted for spasticity, the C7 nerve root of the unaffected arm is cut and transferred to the affected side, where the C7 nerve root is cut and sewn to the C7 from the other side. Recent advances in the surgical approach have allowed to the C7 roots to be directly coapted to to each other in most cases. Because the C7 nerve root from the affected side is cut, the CC7 technique is just as effective at limiting spasticity as a SDR of C7. However, because the working, normal C7 from the unaffected side is connected to the C7 from the affected side, the brain cells from the unaffected normal side are now directly connected to all of the muscles controlled by the C7 nerve root, which include the pectoralis major, latissimus dorsi, teres major, triceps, pronator teres, FDS finger flexors, EDC finger extensors, and ECRB wrist extensor. For patients with limited or no active elbow, wrist, and finger extension, the CC7 can be life changing. The procedure carries a risk of injuring the normal arm, although this is rare and can be overcome with further surgery. Temporary weakness and loss of sensation in the index or long finger are common and can last several months. The procedure is also not universally successful in recovering function, but spasticity control is more reliable.
spasticity 301: ECU to ECRB tendon transfer
The extensor carpi ulnas (ECU) to extensor carp radials brevis (ECRB) transfer can be used to improve grip strength and global hand use in select patients. The ideal candidate should have 1) passive wrist extension beyond 30 degrees, 2) a 4-5/5 MRC strength ECU tendon, 3) inability to actively extend the wrist past neutral, and 4) full or near full active finger extension with the wrist in 30 degrees of extension.
Spasticity 302: Forearm Flexor pronator slide
For children with wrist, finger,and thumb flexor contractures, whether they have some voluntary function of the flexor muscles or not, the most powerful surgery for relaxing the muscles is the flexor-pronator slide. Other options for muscle release, such as fractional lengthening of each individual muscle and z-lengthening of each individual muscle does not provide as much lengthening as a flexor-pronator slide. The procedure requires a full release of the muscle origins of all the volar compartment muscles. The ulnar nerve must be moved with the muscles to prevent stretching of the nerve.
Spasticity 303: Selective Partial Denervation of the forearm, wrist, and hand
For children with spasticity of the wrist flexors (FCR and FCU), the finger flexors (FDS and FDP), the thumb flexor (FPL), and forearm pronators (PT and PQ), but with full passive motion in the forearm, wrist, and hand, selective partial denervation (removal of part of the nerve) may be a better option than muscle and tendon release and lengthening. Some children may have a combination of spasticity and contracture, requiring selective partial denervation and muscle/tendon lengthening. Denervation of approximately 50-80% of the nerve branches to each muscle decreases the spasticity of the muscles without noticeably changing their strength or function in the long term. Some patients experience short term weakness for 3-6 months. The goal is to decrease spasticity without compromising strength. The advantages of selective partial denervation over Botulinum Toxin injections are that the results of the surgery are permanent and do not weaken the target muscles as much.
The technique requires an incision in the proximal forearm just medial to the biceps tendon. The lateral ante brachial cutaneous nerve is identified and protected. The laceratus fibrosis is divided, allowing access to the median nerve. There is commonly at least one nerve branch to the pronator teres, and this is the most proximal branch of the median nerve in the forearm. Next, a common branch to the pronator teres (PT) and flexor carpi radialis (FCR) is encountered. Distal to that is the nerve branch to the flexor digitorum superficialis (FDS). On the deep side of the nerve, typically more lateral, is the anterior interosseous nerve (AIN). The AIN powers the flexor digitorum profundus (FDP) to the index, long, and ring fingers, as well as the small finger in some patients. Each of the branches of the median nerve are isolated and insulated from each other. A nerve stimulator is brought in and used to stimulate each branch, confirming that they are functional. Under magnification, a 0.5-1 cm segment of 50-80% of the working nerves is removed from each muscle. The nerves are stimulated again to confirm that an appropriate amount of nerve has been resected.
The Ulnar nerve is identified through the same incision in the internervous interval between the palmaris longus (PL) and the flexor carpi ulnaris (FCU), which can be identified by a fibrous raphe in the flexor/pronator mass. A nerve stimulator can help differentiate the muscles and identify the interval. The branches to the two heads of the flexor carpi ulnaris (FCU) are identified, as are the typically 2 branches to the FDP to the small and ring fingers. Again, 50-80% of each nerve is resected under magnification.
Because there is nothing to repair other than the skin closure, only a soft dressing is applied and the patient is encouraged to use the arm for light activities. The improvement in spasticity is immediate. Most patients will maintain the improvements from surgery, but recurrence of spasticity is possible. Weakness of the forearm muscles is also a risk, but this is rare.
Spasticity 304: Wrist fusion
When tendon transfers or lengthening are judged to be inadequate to bring the wrist out of flexion, and the child has reached skeletal maturity, a wrist fusion may be considered. Most children, however, respond well to a flexor pronator slide and a wrist fusion is rarely required.
spasticity 305: Elbow release
Elbow flexion contractures are common in patients with spasticity. The spastic muscles that bend the elbow (biceps, brachialis, brachioradialis) limit elbow extension, not allowing the joint capsule, the nerves, the arteries, and the muscles to stretch as the child grows. Preventing a flexion contracture requires frequent stretching exercises and night-time extension splinting. Some children cannot tolerate splinting and/or stretching, making them early candidates for botox injections and casting. If botox and casting cannot resolve the contracture and maintain elbow extension within 30 degrees of full motion, either muscle lengthening or a selective neurectomy should be considered. An elbow release can be more effective and longer lasting than botox injections at controlling flexion contractures. We prefer to do a selective neurectomy rather than a muscle lengthening because the neurectomy directly addresses the spasticity by decreasing the motor drive of the nerves. However, most surgeons are unfamiliar with the neurectomy technique and therefore muscle lengthening remains more popular. There is no data to recommend one technique over the other as yet.
For elbow flexion contractures that are not correctable with sustained passive motion, the only option for obtaining more elbow extension is to lengthen the contracted muscles. This is done through an anterior Z-plasty incision to add skin to the front of the elbow. The biceps is Z-lengthened, the brachialis is fractionally lengthened, and the brachioradialis is myotomized. A cast is applied for 4 weeks in maximal extension and a night splint is worn thereafter.
Separation of a part of a nerve to be removed
The Musculocutaneous Nerve
spasticity 306: Elbow Flexor selective partial denervation
For children with spasticity of the elbow flexors (biceps and brachialis muscles), but with full passive extension of the elbow, selective partial denervation (removal of part of the nerve) may be a better option than an elbow release. Denervation of approximately 50-80% of the nerve branches to the biceps muscle and the brachialis muscle decreases the spasticity of the muscles without noticeably changing their strength or function in the long term. Some patients experience short term weakness in elbow flexion for 3-6 months. The result is an arm the sits extended at rest, but can be brought into flexion when needed, so long as the child has the ability to voluntarily bend the elbow before surgery.
The technique requires identification of the musculocutaneous nerve (MCN) in the medial arm. All of the branches of the MCN that are innervating the biceps and the brachialis are isolated and insulated from each other. A nerve stimulator is brought in and used to stimulate each branch, confirming that they are functional. Under an operative microscope, a 0.5-1 cm segment of 50-80% of the working nerves is removed from each muscle.
Because there is nothing to repair other than the skin closure, only a soft dressing is applied and the patient is encouraged to use the arm for light activities. The improvement in spasticity is immediate. Most patients will maintain the improvements from surgery, but recurrence of spasticity is possible. Weakness of elbow flexion is also a risk, but this is rare.
Spasticity 401: Contralateral C7 Transfer
For patients with severe hemiplegic cerebral palsy, when one arm is normal and the other is severely affected, the contralateral C7 nerve transfer is the most powerful and promising option for both reducing spasticity and for regaining function.
To understand how and why the contralateral C7 nerve transfer works, we have to understand how the nervous system works. There are 3 basic components of the nervous system that create arm movement: the upper motor neuron (in the brain), the lower motor neuron (in the spinal cord), and the muscle. The upper motor neuron is the control center, telling the lower motor neuron what to do. The upper motor neuron also dampens the reflex ark between stretch receptors on the muscles and the lower motor neuron. It is this reflex ark that doctors measure by hitting your knee with a reflex hammer. When the upper motor neuron is injured, as occurs with a stroke, cerebral palsy, or a traumatic brain injury, reflexes are stronger because the lower motor neuron is disinhibited and can fire more freely. This heightened reflex is called spasticity. In order for spasticity to occur, the upper motor neuron has to be injured but the lower motor neuron and the neurons that sense stretch in the muscle must be intact.
When the brain is injured, either from lack of oxygen of from trauma, the upper motor neurons are injured, causing spasticity. The contralateral C7 transfer surgery transfers 20% of the nerves from the functioning arm to the spastic arm. This allows the unaffected side of the brain to control the affected arm. The upper motor neurons and lower motor neurons of the uninjured side are connected to the muscles of the injured arm. This restores the 3 basic components of the nervous system, connecting working upper and lower motor neurons to the muscles. Because a normal reflex arc is restored, spasticity become less severe. Also, because the functioning side of the brain can now control the affected arm, it is possible to gain some active volitional movement in the arm.
Multiple studies and our experience has demonstrated that the risk of injury to the working arm is quite low. Permanent injuries resulting from surgery are rare, but transient weakness in the arm or loss of sensation is common, resolving usually within 2-3 months.